COVID-19 and Gum Disease
As the SAR-CoV-2 virus continues to impact the world, startling new research shows that patients with periodontitis are 9 times more likely to die of coronavirus[1]. Periodontitis, more commonly called gum disease, is one of the most common diseases in the United States. It is estimated that 80% of adults have some level of gum disease. When you combine the new information about coronavirus severity with the sheer prevalence of gum disease, it is worth understanding how these diseases might be related.
Key Points:
- Mouth might be key to transmitting and receiving COVID-19.
- SARS-CoV-2 uses specific proteins to replicate. These proteins are found in higher levels in the mouth.
- Asymptomatic people can transmit the virus via saliva.
- Periodontitis, also called gum disease, may make COVID-19 worse.
- Oral bacteria can spread into your digestive system by swallowing saliva and into your respiratory system when breathing.
- Patients with periodontitis are 9x more likely to die of COVID-19.
- Successful treatment of periodontal disease can lower pathogenic bacteria and inflammation.
Mouth-COVID connection
What role does your mouth play in transmitting and receiving the virus? Studies suggest that the mouth might be the most vulnerable area to this virus due to the abundance of the ACE2 (angiotensin converting enzyme) receptor in the salivary glands, tongue, and tonsils.[2]
The ACE2 receptor is a protein that is normally found on the surface of cells and is found in larger quantities in your mouth. It is also found in the lungs, heart, blood vessels, kidneys, liver and gastrointestinal tract. ACE2 receptors help to generate small proteins by cutting up a larger protein called angiotensinogen. These smaller proteins then help to regulate our cell functions – making sure everything is running smoothly. In particular, proteins from ACE2 help regulate blood pressure, wound healing and inflammation. Inflammation is important and we will talk about it later!
SARS-CoV-2 uses the ACE2 receptor as a gateway into healthy cells. Its ‘spike-like’ protein binds to ACE2, like putting a key in a lock; then the SARS-CoV-2 virus can take over and infect the cell.[3] Since there are more ACE2 receptors found in your mouth – and your mouth is ‘open’ to the virus through air transmission – it makes sense that this area can become a key entry portal for the virus.
Inflammation & Gum Disease
Remember when we said inflammation was important? Inflammation is a normal part of wound healing. When you have a cut, your body tries to fix it by swelling, and moving healing and repair cells to the site of the wound. Molecules called cytokines help the cells communicate, increase inflammation, and stimulate the movement of the healing and repair cells toward the sites of inflammation, infection and trauma.[4]
Guess what – gum disease is an inflammatory disease! Gum disease is your body’s inflammatory response to the bacteria and endotoxins that build up in the oral biofilm.
The sticky stuff on your teeth? That’s the oral biofilm we call plaque; when it isn’t brushed away it hardens into tarter. When tarter builds up on your teeth at the gum line, your gums will become red and puffy. Your body is moving the healing and repair cells to the site to get rid of bacteria and endotoxins. If your body can’t get rid of the bacteria, then chronic inflammation starts. This signals more serious stages of periodontitis. Ligaments and bone holding the tooth in place are destroyed by your immune system and eventually the tooth falls out. Your body will sacrifice an entire tooth to try to get rid of the infection!
Not surprisingly, most dentists have seen a greater number of stress-related oral health issues, including gum disease, among their patients since the start of the pandemic. According to bi-weekly poll by the American Dental Association Health Policy Institute, dentists are reporting a 29.7% increase in periodontal disease.[5] The disease is becoming even more common which means more of us already have inflammation in our bodies.
When Inflammation is Bad
While inflammation is part of your body’s natural wound healing process; inflammation that lasts too long (chronic inflammation) or is too intense can be bad for your body.
With chronic inflammation, the white blood cells can start attacking healthy cells, tissues, and organs. Chronic inflammation is associated with heart disease, diabetes, cancer, arthritis, and bowel diseases like Crohn’s disease and ulcerative colitis.[6]
Even short bursts of inflammation can be bad when they are too intense. During a COVID-19 infection, there can be a very aggressive inflammatory response releasing a large amount of cytokines – those molecules that tell the cells to become inflamed and guide the repair cells (white blood cells) to the site to help healing. When too many cytokines are released at the same time, it is called a “cytokine storm.” Think of this as too many of the messenger cells all yelling at the same time. This results in an excessive inflammatory reaction that can also destroy healthy tissue, healing cells that would normal be helpful become confused and start attacking healthy cells. Cells that should remain in the blood can pass into body tissue (endothelium damage); blood and tissue oxygenation can be reduced (diffuse alveolar damage); and eventually, organs can fail.[7]
In one of the largest cohort studies to date on 5,700 patients who entered the New York hospital system, Richardson et al. (2020) found that the top risk factors of people with severe COVID-19 symptoms included diseases associated with inflammation, such as hypertension (56.6%), obesity (41.7%), and diabetes (33.8%).4
Periodontal disease can increase levels of circulating cytokines in your body. One in particular, called interleukin-6 (IL-6), is one of the key cytokines that leads to the cytokine storm. Elevated interleukin-6 (IL-6) levels can predict if COVID-19 will adversely affect a person’s respiratory system, known as pulmonary complications.[8]
We know too many cytokines are bad – and that both periodontal disease and COVID-19 increase cytokines.
Primed to Spread Disease Throughout the Body
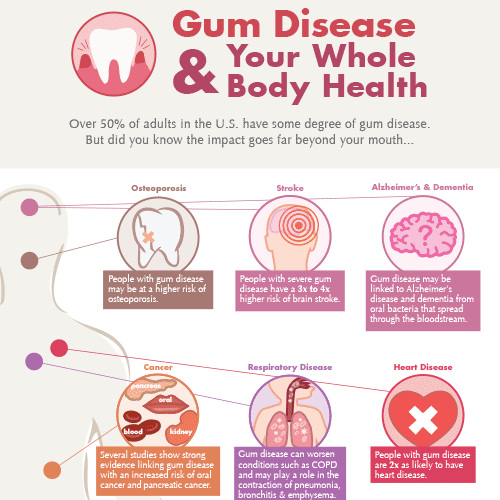
Gum disease has been linked to systemic diseases throughout the body from diabetes, heart disease, cancer, still and pre-term birth, and rheumatoid arthritis, to osteoporosis and obesity. The same bacteria that causes gum disease has even been found in the brain of Alzheimer’s patients.[9] SARS-CoV-2 infection is also associated with an increased incidence of cardiovascular diseases and obesity. [10]
Oral bacteria can spread through your body in three ways. Saliva containing the bacteria can be swallowed and pass through your intestinal system; or inhaled in tiny water droplets within the air you breathe. Periodontal bacteria can even enter your bloodstream through the vascular system in your mouth.
In addition to common inflammatory pathways, a recent review suggests that gum disease may increase COVID-19 severity in other ways.[11]
Professor Mariano Sanz of the Complutense University of Madrid, Spain, one authors of a COVID-Periodontitis severity study in February, noted that oral bacteria in patients with periodontitis can be inhaled and infect the lungs, particularly in those using a ventilator.
Furthermore, respiratory diseases, such as those caused by COVID-19, predispose patients to bacterial superinfections that complicate disease treatment. There is also an increase in viral respiratory infections that spread through contact with mucus from the mouth or nose. 14
Even if you don’t feel sick, new research from March 2021, has proven it is possible for asymptomatic people to transmit the virus to others via saliva.[12] Saliva that contains the virus may help transmitting SARS-CoV-2 to the lungs or digestive system when it is swallowed.
COVID Severity and Gum Disease
The COVID- Periodontitis study found that COVID-19 patients with gum disease 9 times more likely to die, and also that those with gum disease were 3.5 times more likely to be admitted to intensive care and 4.5 times more likely to need a ventilator.
Even before this news was released, other studies showed poor oral health shows a direct connection to COVID-19 infection and to a higher risk of severe illness in patients with COVID-19.[13]
Treating Gum Disease – Helping Lessen COVID?
Studies have shown that periodontal treatment can lower overall systemic inflammatory markers.12 Not all periodontal treatment is the same, and there is a different between ‘treating’ and ‘successfully treating’ the disease.
Eliminating the bacteria triggering the inflammatory response is crucial to successful treatment; and the LANAP protocol is research-proven to immediately suppress periodontal pathogens.[14] If we can reduce pathogenic bacteria and lower inflammation by treating gum disease, can it help to decrease susceptibility to COVID-19 or severity of symptoms?
References
[1] https://onlinelibrary.wiley.com/doi/10.1111/jcpe.13435
[2] https://www.perioimplantadvisory.com/clinical-tips/article/14188402/top-5-oral-manifestations-of-covid19
[3] https://theconversation.com/what-is-the-ace2-receptor-how-is-it-connected-to-coronavirus-and-why-might-it-be-key-to-treating-covid-19-the-experts-explain-136928#:~:text=ACE2%20is%20a%20protein%20on,regulate%20functions%20in%20the%20cell.
[4] https://www.news-medical.net/health/What-are-Cytokines.aspx
[5] https://www.dentistrytoday.com/news/industrynews/item/7045-stress-related-oral-health-issues-see-an-increase-during-the-pandemic?hq_e=el&hq_m=2129211&hq_l=4&hq_v=23c88193a6
[6] https://www.health.harvard.edu/staying-healthy/understanding-acute-and-chronic-inflammation
[7] https://www.frontiersin.org/articles/10.3389/fimmu.2020.01446/full
[8] https://issuu.com/cdapublications/docs/cdapubs_journal_2020_october/s/11067174
[9] https://fightgumdisease.com/total-health/
[10] https://pubmed.ncbi.nlm.nih.gov/33562193/
[11] https://www.nature.com/articles/s41415-020-1747-8
[12] https://www.nature.com/articles/s41591-021-01296-8
[13] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7303044/
[14] https://www.lanap.com/wp-content/uploads/2018/10/McCawley-et-al-2018-LANAP-immediate-micro-effects.pdf